[read time: 4 min approx.]
Words written by Ken Eastwood
For over a decade, Associate Professor Carlos Salomon Gallo has been searching for new and better ways to detect ovarian cancer sooner. Some of the latest exciting results in this quest, which has been funded in part by the Ovarian Cancer Research Foundation and the Australian Government’s Medical Research Future Fund, were recently published in the American Chemical Society’s journal ACS Nano and The Journal of Bioinformatics.
Associate Professor Salomon Gallo, who is group leader of the Translational Extracellular Vesicles in Obstetrics and Gynae-Oncology Group at The University of Queensland Centre for Clinical Research (UQCCR), explains his work and how it is progressing.
What is the biggest problem with diagnosing ovarian cancer?
Every day in Australia, three women die from ovarian cancer – that’s one every eight hours. The disease is often diagnosed in the late stages, which contributes to a low five-year survival rate of just 49%. But we know that if we can identify women in the early stages of the disease, their five-year survival rate is around 90%. The main problem is how you can identify these women in the earliest stage, when the early stages don’t have consistent symptoms. Some of the symptoms are abdominal pain or back problems – it could be 100 million different things – and the women find out later that they’ve got ovarian cancer.
What we’ve been working on for several years is identifying a molecular signature for ovarian cancer in the blood of women – a simple blood test. The existing gold standard test, CA-125, is quite good at detecting late-stage ovarian cancer, but levels are only elevated in about 50% of early-stage cases, which means for early detection it is about as reliable as flipping a coin.
 Pictured: Associate Professor Carlos Salomon, Head of the Translational Extracellular Vesicles in Obstetrics and Gynae-Oncology Group, Dr Soumyalekshmi Nair (Theme Leader, Therapeutics)
Pictured: Associate Professor Carlos Salomon, Head of the Translational Extracellular Vesicles in Obstetrics and Gynae-Oncology Group, Dr Soumyalekshmi Nair (Theme Leader, Therapeutics)
How have you approached providing an alternative ovarian cancer early detection method?
Humans have a gene called p53 that can identify when DNA is damaged and activates genes to fix the damage. Sort of like the gene police, p53 identifies the bad guys. It usually functions really well, but if it is mutated itself, it can’t do its job to stop cancer cells from growing and proliferating.
More than 95 per cent of women with high-grade serous ovarian cancer have a p53 mutation. Their immune systems generate autoantibodies against the mutation, and these circulate in the blood. In ovarian cancer, the increasing amount of these autoantibodies is directly associated with progression of the disease. This presents an opportunity to potentially detect ovarian cancer earlier, as well as better evaluate the progression of the disease.
In collaboration with Professor Yusuke Yamauchi from the Australian Institute for Bioengineering and Nanotechnology (AIBN), we have developed a way to detect and measure the quantities of these autoantibodies, and our test can now detect the disease at concentration levels 50 times lower than the existing commercial kit — being able to detect in lower concentrations means being able to detect earlier. Our method not only gives us a great head start in detecting ovarian cancer earlier but also in evaluating the progression of the disease.
To prove this further, we are looking to start a new study in a larger population of women (around 200 women).
Can the P53 test be used for anything else?
We believe that the p53 mutation can not only be used for early detection of ovarian cancer but could also be used as a marker to show how women are responding to chemotherapy. There are currently no tests available to identify a woman’s responsiveness or chemoresistance, but the level of p53 autoantibodies in their blood could give an indication as to whether these women respond better to certain drugs than others.
A p53 test could also potentially detect the majority of cancers, not just ovarian cancer. Colorectal cancer could potentially be our next target, but at the moment we are optimising the test for ovarian cancer.
If a simple blood test to detect early ovarian cancer could be manufactured, how would it be distributed or made available?
While we’re working on finding a solution, those sorts of questions need to be looked into by policy makers, depending on the outcomes of several biomarker trials. If an easy test is developed, should we screen all women for ovarian cancer after a certain age?
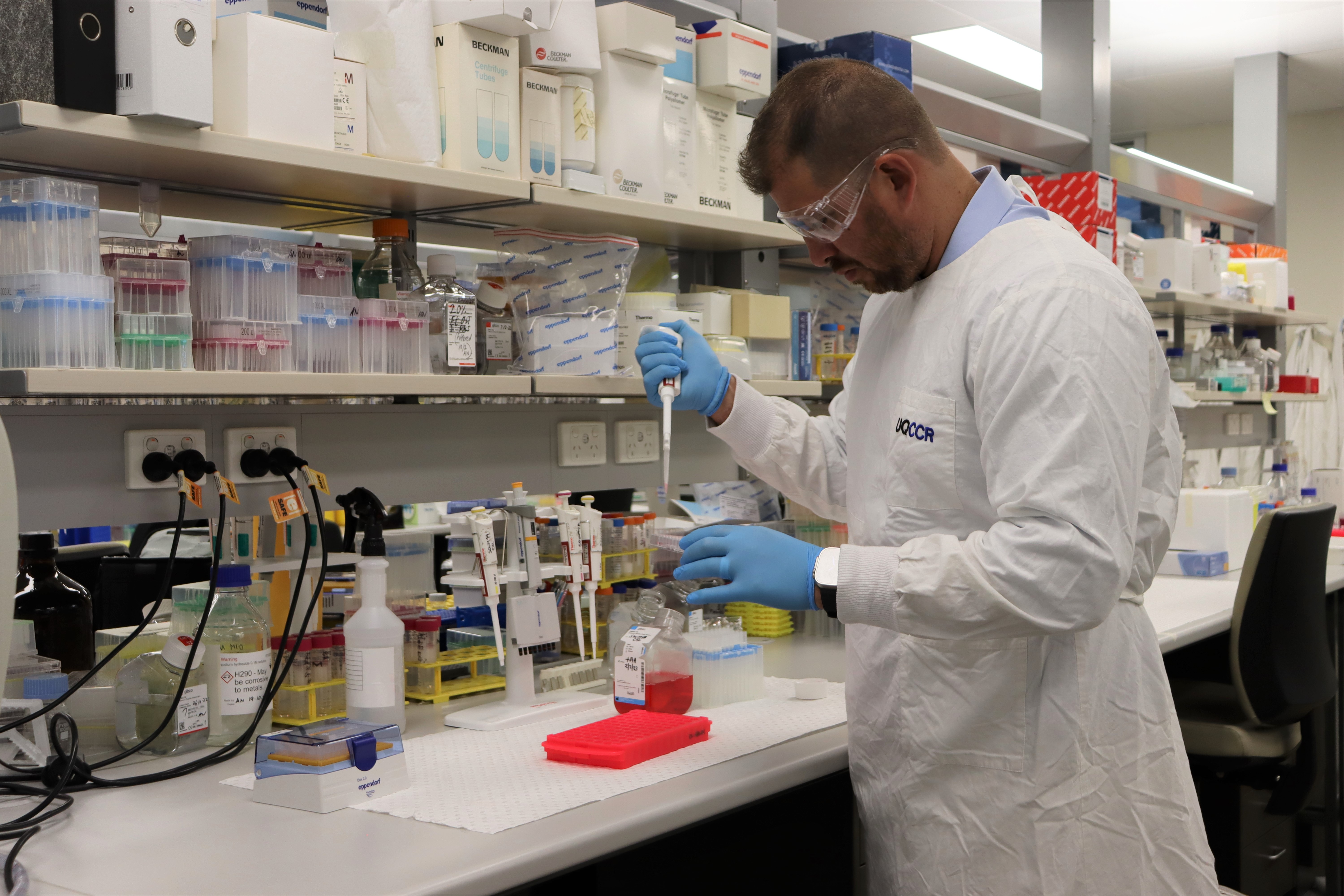 Pictured: Associate Professor Carlos Salomon, Head of the Translational Extracellular Vesicles in Obstetrics and Gynae-Oncology Group
Pictured: Associate Professor Carlos Salomon, Head of the Translational Extracellular Vesicles in Obstetrics and Gynae-Oncology Group
You’ve also been developing another possible solution to the early diagnosis of ovarian cancer. What is that?
Yes, we’ve advanced in the steps and processes for implementing a new In Vitro Diagnostic Multivariate Index Assay for the early detection of ovarian cancer and completed the discovery stages of this test including defining the intended use and updating the diagnostic algorithm. Thus, we are hoping to begin the implementation process, for clinical application, in about five years.
It’s called OCRF-7, because the OCRF was the first not-for-profit organisation to support our research into a signature based in proteins which are found in the blood. We looked at about 3000 variables, and developed a biomarker based on seven of those – the different quantities of those seven markers give us an accurate way of detecting ovarian cancer.
We tested it initially using the records and blood samples of 150 women, then 465 women, and now have funding to test it in a group of 3000 samples. So far, we’ve shown it has over 90 per cent classification efficiency in detecting early-stage ovarian cancer. That’s significantly better than around 60 per cent for the existing CA125 test.
.png) Pictured: Associate Professor Carlos Salomon, Head of the Translational Extracellular Vesicles in Obstetrics and Gynae-Oncology Group, Dr Soumyalekshmi Nair (Theme Leader, Therapeutics), Dr Andrew Lai (Theme Leader, Proteomics), and Dr Dominic Guanzon (Theme Leader, Genomics).
Pictured: Associate Professor Carlos Salomon, Head of the Translational Extracellular Vesicles in Obstetrics and Gynae-Oncology Group, Dr Soumyalekshmi Nair (Theme Leader, Therapeutics), Dr Andrew Lai (Theme Leader, Proteomics), and Dr Dominic Guanzon (Theme Leader, Genomics).
Are there many people working on this?
There’s a huge multidisciplinary team aligned behind a common goal to win the fight against ovarian cancer. At The University of Queensland (UQ) there are around 25 people involved, including Professor Yusuke Yamauchi, and Dr Mostafa Masud (first author of the study published at American Chemical Society’s journal ACS Nano) from the AIBN within UQ. But there are other people at the Australian National University in Canberra, Mater Research and The University of Sydney, as well as teams in the UK and Singapore.
From small seeds big things grow. After having funded Carlos’ research in this space for several years, its truly exciting for the OCRF to see the promise his multi-pronged approaches to early detection are producing. With his research now receiving government funding it is evolving, with significant clinical trials on the horizon. The OCRF plays a vital role in identifying promising early-stage research and funding projects to become important clinical trials like Carlos’— ultimately to provide an early detection solution for ovarian cancer.
Support projects like Carlos’ by donating to the OCRF.
This article has been reviewed and approved by Associate Professor Carlos Salomon Gallo.